Abstract
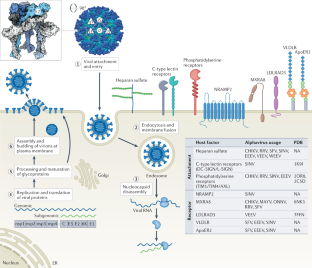
Alphaviruses are arthropod-transmitted RNA viruses that cause epidemics of human infection and disease on a global scale. These viruses are classified as either arthritogenic or encephalitic based on their genetic relatedness and the clinical syndromes they cause. Although there are currently no approved therapeutics or vaccines against alphaviruses, passive transfer of monoclonal antibodies confers protection in animal models. This Review highlights recent advances in our understanding of the host factors required for alphavirus entry, the mechanisms of action by which protective antibodies inhibit different steps in the alphavirus infection cycle and candidate alphavirus vaccines currently under clinical evaluation that focus on humoral immunity. A comprehensive understanding of alphavirus entry and antibody-mediated protection may inform the development of new classes of countermeasures for these emerging viruses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to Journal
Get full journal access for 1 year
99,00 €
only 8,25 € per issue
Tax calculation will be finalised during checkout.
Buy article
Get time limited or full article access on ReadCube.
$32.00
All prices are NET prices.

References
-
Suhrbier, A., Jaffar-Bandjee, M. C. & Gasque, P. Arthritogenic alphaviruses — an overview. Nat. Rev. Rheumatol. 8, 420–429 (2012).
-
Carrera, J. P. et al. Eastern equine encephalitis in Latin America. N. Engl. J. Med. 369, 732–744 (2013).
-
Morens, D. M., Folkers, G. K. & Fauci, A. S. Eastern equine encephalitis virus — another emergent arbovirus in the United States. N. Engl. J. Med. 381, 1989–1992 (2019).
-
Baker, R. E. et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 20, 193–205 (2022).
-
Weaver, S. C. & Reisen, W. K. Present and future arboviral threats. Antivir. Res. 85, 328–345 (2010).
-
Schuffenecker, I. et al. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med. 3, e263 (2006).
-
Rezza, G. Dengue and chikungunya: long-distance spread and outbreaks in naive areas. Pathog. Glob. Health 108, 349–355 (2014).
-
Harley, D., Sleigh, A. & Ritchie, S. Ross River virus transmission, infection, and disease: a cross-disciplinary review. Clin. Microbiol. Rev. 14, 909–932 (2001).
-
Aguilar-Luis, M. A. et al. An emerging public health threat: Mayaro virus increases its distribution in Peru. Int. J. Infect. Dis. 92, 253–258 (2020).
-
Sidwell, R. W. & Smee, D. F. Viruses of the Bunya- and Togaviridae families: potential as bioterrorism agents and means of control. Antivir. Res. 57, 101–111 (2003).
-
Weaver, S. C. et al. Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. VEE Study Group. Lancet 348, 436–440 (1996).
-
Torres-Ruesta, A., Chee, R. S. & Ng, L. F. P. Insights into antibody-mediated alphavirus immunity and vaccine development landscape. Microorganisms https://doi.org/10.3390/microorganisms9050899 (2021).
-
Kafai, N. M., Diamond, M. S. & Fox, J. M. Distinct cellular tropism and immune responses to alphavirus infection. Annu. Rev. Immunol. 40, 615–649 (2022).
-
Holmes, A. C., Basore, K., Fremont, D. H. & Diamond, M. S. A molecular understanding of alphavirus entry. PLoS Pathog. 16, e1008876 (2020).
-
Voss, J. E. et al. Glycoprotein organization of chikungunya virus particles revealed by X-ray crystallography. Nature 468, 709–712 (2010).
-
Li, L., Jose, J., Xiang, Y., Kuhn, R. J. & Rossmann, M. G. Structural changes of envelope proteins during alphavirus fusion. Nature 468, 705–708 (2010).
-
Snyder, J. E. et al. Functional characterization of the alphavirus TF protein. J. Virol. 87, 8511–8523 (2013).
-
Jose, J., Snyder, J. E. & Kuhn, R. J. A structural and functional perspective of alphavirus replication and assembly. Fut. Microbiol. 4, 837–856 (2009).
-
Hasan, S. S. et al. Cryo-EM structures of Eastern equine encephalitis virus reveal mechanisms of virus disassembly and antibody neutralization. Cell Rep. 25, 3136–3147.e5 (2018).
-
Basore, K. et al. Cryo-EM structure of chikungunya virus in complex with the Mxra8 receptor. Cell 177, 1725–1737.e16 (2019).
-
Zhang, X., Fugere, M., Day, R. & Kielian, M. Furin processing and proteolytic activation of Semliki Forest virus. J. Virol. 77, 2981–2989 (2003).
-
de Curtis, I. & Simons, K. Dissection of Semliki Forest virus glycoprotein delivery from the trans-Golgi network to the cell surface in permeabilized BHK cells. Proc. Natl Acad. Sci. USA 85, 8052–8056 (1988).
-
Uchime, O., Fields, W. & Kielian, M. The role of E3 in pH protection during alphavirus assembly and exit. J. Virol. 87, 10255–10262 (2013).
-
Sjöberg, M., Lindqvist, B. & Garoff, H. Activation of the alphavirus spike protein is suppressed by bound E3. J. Virol. 85, 5644–5650 (2011).
-
Snyder, A. J. & Mukhopadhyay, S. The alphavirus E3 glycoprotein functions in a clade-specific manner. J. Virol. 86, 13609–13620 (2012).
-
Chen, L. et al. Implication for alphavirus host-cell entry and assembly indicated by a 3.5A resolution cryo-EM structure. Nat. Commun. 9, 5326 (2018).
-
Davis, N. L., Pence, D. F., Meyer, W. J., Schmaljohn, A. L. & Johnston, R. E. Alternative forms of a strain-specific neutralizing antigenic site on the Sindbis virus E2 glycoprotein. Virology 161, 101–108 (1987).
-
Flynn, D. C., Olmsted, R. A., Mackenzie, J. M. Jr & Johnston, R. E. Antibody-mediated activation of Sindbis virus. Virology 166, 82–90 (1988).
-
Meyer, W. J. & Johnston, R. E. Structural rearrangement of infecting Sindbis virions at the cell surface: mapping of newly accessible epitopes. J. Virol. 67, 5117–5125 (1993).
-
Smith, T. J. et al. Putative receptor binding sites on alphaviruses as visualized by cryoelectron microscopy. Proc. Natl Acad. Sci. USA 92, 10648–10652 (1995).
-
Mukhopadhyay, S. et al. Mapping the structure and function of the E1 and E2 glycoproteins in alphaviruses. Structure 14, 63–73 (2006).
-
Ubol, S. & Griffin, D. E. Identification of a putative alphavirus receptor on mouse neural cells. J. Virol. 65, 6913–6921 (1991).
-
Vrati, S., Kerr, P. J., Weir, R. C. & Dalgarno, L. Entry kinetics and mouse virulence of Ross River virus mutants altered in neutralization epitopes. J. Virol. 70, 1745–1750 (1996).
-
Song, H. et al. Molecular basis of arthritogenic alphavirus receptor MXRA8 binding to chikungunya virus envelope protein. Cell 177, 1714–1724.e12 (2019).
-
Zhang, R. et al. Mxra8 is a receptor for multiple arthritogenic alphaviruses. Nature 557, 570–574 (2018).
-
Ramsey, J. & Mukhopadhyay, S. Disentangling the frames, the state of research on the alphavirus 6K and TF proteins. Viruses https://doi.org/10.3390/v9080228 (2017).
-
Loewy, A., Smyth, J., von Bonsdorff, C. H., Liljestrom, P. & Schlesinger, M. J. The 6-kilodalton membrane protein of Semliki Forest virus is involved in the budding process. J. Virol. 69, 469–475 (1995).
-
Lescar, J. et al. The fusion glycoprotein shell of Semliki Forest virus: an icosahedral assembly primed for fusogenic activation at endosomal pH. Cell 105, 137–148 (2001).
-
Roussel, A. et al. Structure and interactions at the viral surface of the envelope protein E1 of Semliki Forest virus. Structure 14, 75–86 (2006).
-
Gibbons, D. L. et al. Visualization of the target-membrane-inserted fusion protein of Semliki Forest virus by combined electron microscopy and crystallography. Cell 114, 573–583 (2003).
-
Gibbons, D. L. et al. Conformational change and protein-protein interactions of the fusion protein of Semliki Forest virus. Nature 427, 320–325 (2004).
-
Jin, J. et al. Neutralizing antibodies inhibit chikungunya virus budding at the plasma membrane. Cell Host Microbe 24, 417–428.e5 (2018).
-
Soonsawad, P. et al. Structural evidence of glycoprotein assembly in cellular membrane compartments prior to alphavirus budding. J. Virol. 84, 11145–11151 (2010).
-
Jose, J., Taylor, A. B. & Kuhn, R. J. Spatial and temporal analysis of alphavirus replication and assembly in mammalian and mosquito cells. mBio https://doi.org/10.1128/mBio.02294-16 (2017).
-
Silva, L. A. et al. A single-amino-acid polymorphism in chikungunya virus e2 glycoprotein influences glycosaminoglycan utilization. J. Virol. 88, 2385–2397 (2014).
-
Tanaka, A. et al. Genome-wide screening uncovers the significance of N-sulfation of heparan sulfate as a host cell factor for chikungunya virus infection. J. Virol. https://doi.org/10.1128/jvi.00432-17 (2017).
-
Zhang, W., Heil, M., Kuhn, R. J. & Baker, T. S. Heparin binding sites on Ross River virus revealed by electron cryo-microscopy. Virology 332, 511–518 (2005).
-
Byrnes, A. P. & Griffin, D. E. Binding of Sindbis virus to cell surface heparan sulfate. J. Virol. 72, 7349–7356 (1998).
-
Gardner, C. L., Ebel, G. D., Ryman, K. D. & Klimstra, W. B. Heparan sulfate binding by natural Eastern equine encephalitis viruses promotes neurovirulence. Proc. Natl Acad. Sci. USA 108, 16026–16031 (2011).
-
Gardner, C. L. et al. Natural variation in the heparan sulfate binding domain of the Eastern equine encephalitis virus E2 glycoprotein alters interactions with cell surfaces and virulence in mice. J. Virol. 87, 8582–8590 (2013).
-
Bernard, K. A., Klimstra, W. B. & Johnston, R. E. Mutations in the E2 glycoprotein of Venezuelan equine encephalitis virus confer heparan sulfate interaction, low morbidity, and rapid clearance from blood of mice. Virology 276, 93–103 (2000).
-
Klimstra, W. B., Ryman, K. D. & Johnston, R. E. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J. Virol. 72, 7357–7366 (1998).
-
Ashbrook, A. W. et al. Residue 82 of the chikungunya virus E2 attachment protein modulates viral dissemination and arthritis in mice. J. Virol. 88, 12180–12192 (2014).
-
Klimstra, W. B., Nangle, E. M., Smith, M. S., Yurochko, A. D. & Ryman, K. D. DC-SIGN and L-SIGN can act as attachment receptors for alphaviruses and distinguish between mosquito cell- and mammalian cell-derived viruses. J. Virol. 77, 12022–12032 (2003).
-
Feinberg, H., Mitchell, D. A., Drickamer, K. & Weis, W. I. Structural basis for selective recognition of oligosaccharides by DC-SIGN and DC-SIGNR. Science 294, 2163–2166 (2001).
-
Jemielity, S. et al. TIM-family proteins promote infection of multiple enveloped viruses through virion-associated phosphatidylserine. PLoS Pathog. 9, e1003232 (2013).
-
Moller-Tank, S., Kondratowicz, A. S., Davey, R. A., Rennert, P. D. & Maury, W. Role of the phosphatidylserine receptor TIM-1 in enveloped-virus entry. J. Virol. 87, 8327–8341 (2013).
-
Kirui, J. et al. The phosphatidylserine receptor TIM-1 enhances authentic chikungunya virus cell entry. Cells https://doi.org/10.3390/cells10071828 (2021).
-
Wang, K. S., Kuhn, R. J., Strauss, E. G., Ou, S. & Strauss, J. H. High-affinity laminin receptor is a receptor for Sindbis virus in mammalian cells. J. Virol. 66, 4992–5001 (1992).
-
Ludwig, G. V., Kondig, J. P. & Smith, J. F. A putative receptor for Venezuelan equine encephalitis virus from mosquito cells. J. Virol. 70, 5592–5599 (1996).
-
Wintachai, P. et al. Identification of prohibitin as a chikungunya virus receptor protein. J. Med. Virol. 84, 1757–1770 (2012).
-
De Caluwé, L. et al. The CD147 protein complex is involved in entry of chikungunya virus and related alphaviruses in human cells. Front. Microbiol. 12, 615165 (2021).
-
Helenius, A. et al. Human (HLA-A and HLA-B) and murine (H-2K and H-2D) histocompatibility antigens are cell surface receptors for Semliki Forest virus. Proc. Natl Acad. Sci. USA 75, 3846–3850 (1978).
-
Rose, P. P. et al. Natural resistance-associated macrophage protein is a cellular receptor for Sindbis virus in both insect and mammalian hosts. Cell Host Microbe 10, 97–104 (2011).
-
Kim, A. S. et al. An evolutionary insertion in the Mxra8 receptor-binding site confers resistance to alphavirus infection and pathogenesis. Cell Host Microbe 27, 428–440.e9 (2020).
-
Zhang, R. et al. Expression of the Mxra8 receptor promotes alphavirus infection and pathogenesis in mice and Drosophila. Cell Rep. 28, 2647–2658.e5 (2019).
-
Ma, H. et al. LDLRAD3 is a receptor for Venezuelan equine encephalitis virus. Nature 588, 308–314 (2020).
-
Basore, K. et al. Structure of Venezuelan equine encephalitis virus in complex with the LDLRAD3 receptor. Nature 598, 672–676 (2021).
-
Ma, B., Huang, C., Ma, J., Xiang, Y. & Zhang, X. Structure of Venezuelan equine encephalitis virus with its receptor LDLRAD3. Nature 598, 677–681 (2021).
-
Clark, L. E. et al. VLDLR and ApoER2 are receptors for multiple alphaviruses. Nature 602, 475–480 (2022).
-
Levin, M. J. et al. Intramuscular AZD7442 (tixagevimab–cilgavimab) for prevention of Covid-19. N. Engl. J. Med. 386, 2188–2200 (2022).
-
Gupta, A. et al. Early treatment for Covid-19 with SARS-CoV-2 neutralizing antibody sotrovimab. N. Engl. J. Med. 385, 1941–1950 (2021).
-
Robbie, G. J. et al. A novel investigational Fc-modified humanized monoclonal antibody, motavizumab-YTE, has an extended half-life in healthy adults. Antimicrob. Agents Chemother. 57, 6147–6153 (2013).
-
Boere, W. A., Benaissa-Trouw, B. J., Harmsen, M., Kraaijeveld, C. A. & Snippe, H. Neutralizing and non-neutralizing monoclonal antibodies to the E2 glycoprotein of Semliki Forest virus can protect mice from lethal encephalitis. J. Gen. Virol. 64, 1405–1408 (1983).
-
Boere, W. A. et al. Identification of distinct antigenic determinants on Semliki Forest virus by using monoclonal antibodies with different antiviral activities. J. Virol. 52, 575–582 (1984).
-
Stanley, J., Cooper, S. J. & Griffin, D. E. Alphavirus neurovirulence: monoclonal antibodies discriminating wild-type from neuroadapted Sindbis virus. J. Virol. 56, 110–119 (1985).
-
Stec, D. S., Waddell, A., Schmaljohn, C. S., Cole, G. A. & Schmaljohn, A. L. Antibody-selected variation and reversion in Sindbis virus neutralization epitopes. J. Virol. 57, 715–720 (1986).
-
Vrati, S., Fernon, C. A., Dalgarno, L. & Weir, R. C. Location of a major antigenic site involved in Ross River virus neutralization. Virology 162, 346–353 (1988).
-
Roehrig, J. T., Day, J. W. & Kinney, R. M. Antigenic analysis of the surface glycoproteins of a Venezuelan equine encephalomyelitis virus (TC-83) using monoclonal antibodies. Virology 118, 269–278 (1982).
-
Roehrig, J. T., Gorski, D. & Schlesinger, M. J. Properties of monoclonal antibodies directed against the glycoproteins of Sindbis virus. J. Gen. Virol. 59, 421–425 (1982).
-
Roehrig, J. T. & Mathews, J. H. The neutralization site on the E2 glycoprotein of Venezuelan equine encephalomyelitis (TC-83) virus is composed of multiple conformationally stable epitopes. Virology 142, 347–356 (1985).
-
Mayne, J. T., Rice, C. M., Strauss, E. G., Hunkapiller, M. W. & Strauss, J. H. Biochemical studies of the maturation of the small Sindbis virus glycoprotein E3. Virology 134, 338–357 (1984).
-
Parker, M. D. et al. Antibody to the E3 glycoprotein protects mice against lethal Venezuelan equine encephalitis virus infection. J. Virol. 84, 12683–12690 (2010).
-
Warter, L. et al. Chikungunya virus envelope-specific human monoclonal antibodies with broad neutralization potency. J. Immunol. 186, 3258–3264 (2011).
-
Pal, P. et al. Development of a highly protective combination monoclonal antibody therapy against chikungunya virus. PLoS Pathog. 9, e1003312 (2013).
-
Fox, J. M. et al. Broadly neutralizing alphavirus antibodies bind an epitope on E2 and inhibit entry and egress. Cell 163, 1095–1107 (2015).
-
Smith, S. A. et al. Isolation and characterization of broad and ultrapotent human monoclonal antibodies with therapeutic activity against chikungunya virus. Cell Host Microbe 18, 86–95 (2015).
-
Fong, R. H. et al. Exposure of epitope residues on the outer face of the chikungunya virus envelope trimer determines antibody neutralizing efficacy. J. Virol. 88, 14364–14379 (2014).
-
Quiroz, J. A. et al. Human monoclonal antibodies against chikungunya virus target multiple distinct epitopes in the E1 and E2 glycoproteins. PLoS Pathog. 15, e1008061 (2019).
-
Malonis, R. J. et al. Near-germline human monoclonal antibodies neutralize and protect against multiple arthritogenic alphaviruses. Proc. Natl Acad. Sci. USA https://doi.org/10.1073/pnas.2100104118 (2021).
-
Goh, L. Y. et al. Neutralizing monoclonal antibodies to the E2 protein of chikungunya virus protects against disease in a mouse model. Clin. Immunol. 149, 487–497 (2013).
-
Powell, L. A. et al. Human monoclonal antibodies against Ross River virus target epitopes within the E2 protein and protect against disease. PLoS Pathog. 16, e1008517 (2020).
-
Powell, L. A. et al. Human mAbs broadly protect against arthritogenic alphaviruses by recognizing conserved elements of the Mxra8 receptor-binding site. Cell Host Microbe 28, 699–711.e7 (2020).
-
Earnest, J. T. et al. Neutralizing antibodies against Mayaro virus require Fc effector functions for protective activity. J. Exp. Med. 216, 2282–2301 (2019).
-
Kim, A. S. et al. Protective antibodies against Eastern equine encephalitis virus bind to epitopes in domains A and B of the E2 glycoprotein. Nat. Microbiol. 4, 187–197 (2019).
-
Williamson, L. E. et al. Human antibodies protect against aerosolized Eastern equine encephalitis virus infection. Cell 183, 1884–1900.e23 (2020).
-
Liu, J. L., Shriver-Lake, L. C., Zabetakis, D., Goldman, E. R. & Anderson, G. P. Selection of single-domain antibodies towards Western equine encephalitis virus. Antibodies https://doi.org/10.3390/antib7040044 (2018).
-
Kafai, N. M. et al. Neutralizing antibodies protect mice against Venezuelan equine encephalitis virus aerosol challenge. J. Exp. Med. https://doi.org/10.1084/jem.20212532 (2022).
-
Porta, J. et al. Locking and blocking the viral landscape of an alphavirus with neutralizing antibodies. J. Virol. 88, 9616–9623 (2014).
-
Sun, S. et al. Structural analyses at pseudo atomic resolution of chikungunya virus and antibodies show mechanisms of neutralization. eLife 2, e00435 (2013).
-
Johnston, R. E. & Smith, J. F. Selection for accelerated penetration in cell culture coselects for attenuated mutants of Venezuelan equine encephalitis virus. Virology 162, 437–443 (1988).
-
Russell, D. L., Dalrymple, J. M. & Johnston, R. E. Sindbis virus mutations which coordinately affect glycoprotein processing, penetration, and virulence in mice. J. Virol. 63, 1619–1629 (1989).
-
Pence, D. F., Davis, N. L. & Johnston, R. E. Antigenic and genetic characterization of Sindbis virus monoclonal antibody escape mutants which define a pathogenesis domain on glycoprotein E2. Virology 175, 41–49 (1990).
-
Pal, P. et al. Chikungunya viruses that escape monoclonal antibody therapy are clinically attenuated, stable, and not purified in mosquitoes. J. Virol. 88, 8213–8226 (2014).
-
EnCheng, S. et al. Analysis of murine B-cell epitopes on Eastern equine encephalitis virus glycoprotein E2. Appl. Microbiol. Biotechnol. 97, 6359–6372 (2013).
-
Agapov, E. V. et al. Localization of four antigenic sites involved in Venezuelan equine encephalomyelitis virus protection. Arch. Virol. 139, 173–181 (1994).
-
Earnest, J. T. et al. The mechanistic basis of protection by non-neutralizing anti-alphavirus antibodies. Cell Rep. 35, 108962 (2021).
-
Lu, L. L., Suscovich, T. J., Fortune, S. M. & Alter, G. Beyond binding: antibody effector functions in infectious diseases. Nat. Rev. Immunol. 18, 46–61 (2018).
-
Tao, M. H. & Morrison, S. L. Studies of aglycosylated chimeric mouse-human IgG. Role of carbohydrate in the structure and effector functions mediated by the human IgG constant region. J. Immunol. 143, 2595–2601 (1989).
-
Després, P., Griffin, J. W. & Griffin, D. E. Effects of anti-E2 monoclonal antibody on Sindbis virus replication in AT3 cells expressing bcl-2. J. Virol. 69, 7006–7014 (1995).
-
Levine, B. et al. Antibody-mediated clearance of alphavirus infection from neurons. Science 254, 856–860 (1991).
-
Navaratnarajah, C. K. & Kuhn, R. J. Functional characterization of the Sindbis virus E2 glycoprotein by transposon linker-insertion mutagenesis. Virology 363, 134–147 (2007).
-
Fox, J. M. et al. A cross-reactive antibody protects against Ross River virus musculoskeletal disease despite rapid neutralization escape in mice. PLoS Pathog. 16, e1008743 (2020).
-
Lee, C. Y. et al. Chikungunya virus neutralization antigens and direct cell-to-cell transmission are revealed by human antibody-escape mutants. PLoS Pathog. 7, e1002390 (2011).
-
Strauss, E. G., Stec, D. S., Schmaljohn, A. L. & Strauss, J. H. Identification of antigenically important domains in the glycoproteins of Sindbis virus by analysis of antibody escape variants. J. Virol. 65, 4654–4664 (1991).
-
Roehrig, J. T. et al. Identification of monoclonal antibodies capable of differentiating antigenic varieties of Eastern equine encephalitis viruses. Am. J. Trop. Med. Hyg. 42, 394–398 (1990).
-
Mendoza, Q. P., Stanley, J. & Griffin, D. E. Monoclonal antibodies to the E1 and E2 glycoproteins of Sindbis virus: definition of epitopes and efficiency of protection from fatal encephalitis. J. Gen. Virol. 69, 3015–3022 (1988).
-
Schmaljohn, A. L., Johnson, E. D., Dalrymple, J. M. & Cole, G. A. Non-neutralizing monoclonal antibodies can prevent lethal alphavirus encephalitis. Nature 297, 70–72 (1982).
-
Schmaljohn, A. L., Kokubun, K. M. & Cole, G. A. Protective monoclonal antibodies define maturational and pH-dependent antigenic changes in Sindbis virus E1 glycoprotein. Virology 130, 144–154 (1983).
-
Stanley, J., Cooper, S. J. & Griffin, D. E. Monoclonal antibody cure and prophylaxis of lethal Sindbis virus encephalitis in mice. J. Virol. 58, 107–115 (1986).
-
Kim, A. S. et al. Pan-protective anti-alphavirus human antibodies target a conserved E1 protein epitope. Cell 184, 4414–4429.e19 (2021).
-
Williamson, L. E. et al. Therapeutic alphavirus cross-reactive E1 human antibodies inhibit viral egress. Cell 184, 4430–4446.e22 (2021).
-
Calvert, A. E. et al. Exposing cryptic epitopes on the Venezuelan equine encephalitis virus E1 glycoprotein prior to treatment with alphavirus cross-reactive monoclonal antibody allows blockage of replication early in infection. Virology 565, 13–21 (2022).
-
Fox, J. M. et al. Optimal therapeutic activity of monoclonal antibodies against chikungunya virus requires Fc-FcγR interaction on monocytes. Sci. Immunol. https://doi.org/10.1126/sciimmunol.aav5062 (2019).
-
Tuekprakhon, A. et al. Broad-spectrum monoclonal antibodies against chikungunya virus structural proteins: promising candidates for antibody-based rapid diagnostic test development. PLoS ONE 13, e0208851 (2018).
-
Marston, H. D., Paules, C. I. & Fauci, A. S. Monoclonal antibodies for emerging infectious diseases — borrowing from history. N. Engl. J. Med. 378, 1469–1472 (2018).
-
Simoes, E. A. et al. Palivizumab prophylaxis, respiratory syncytial virus, and subsequent recurrent wheezing. J. Pediatr. 151, 34–42 (2007).
-
Zost, S. J. et al. Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature 584, 443–449 (2020).
-
Pinto, D. et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature 583, 290–295 (2020).
-
Broeckel, R. et al. Therapeutic administration of a recombinant human monoclonal antibody reduces the severity of chikungunya virus disease in rhesus macaques. PLoS Negl. Trop. Dis. 11, e0005637 (2017).
-
Burke, C. W. et al. Therapeutic monoclonal antibody treatment protects nonhuman primates from severe Venezuelan equine encephalitis virus disease after aerosol exposure. PLoS Pathog. 15, e1008157 (2019).
-
Kose, N. et al. A lipid-encapsulated mRNA encoding a potently neutralizing human monoclonal antibody protects against chikungunya infection. Sci. Immunol. https://doi.org/10.1126/sciimmunol.aaw6647 (2019).
-
August, A. et al. A phase 1 trial of lipid-encapsulated mRNA encoding a monoclonal antibody with neutralizing activity against chikungunya virus. Nat. Med. 27, 2224–2233 (2021).
-
Corbett, K. S. et al. Evaluation of the mRNA-1273 vaccine against SARS-CoV-2 in nonhuman primates. N. Engl. J. Med. 383, 1544–1555 (2020).
-
Gorchakov, R. et al. Attenuation of chikungunya virus vaccine strain 181/clone 25 is determined by two amino acid substitutions in the E2 envelope glycoprotein. J. Virol. 86, 6084–6096 (2012).
-
Edelman, R. et al. Phase II safety and immunogenicity study of live chikungunya virus vaccine TSI-GSD-218. Am. J. Trop. Med. Hyg. 62, 681–685 (2000).
-
Pittman, P. R. et al. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine 14, 337–343 (1996).
-
Paessler, S. et al. Recombinant Sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. J. Virol. 77, 9278–9286 (2003).
-
Paessler, S. et al. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J. Virol. 80, 2784–2796 (2006).
-
Rossi, S. L. et al. IRES-containing VEEV vaccine protects cynomolgus macaques from IE Venezuelan equine encephalitis virus aerosol challenge. PLoS Negl. Trop. Dis. 9, e0003797 (2015).
-
Trobaugh, D. W., Sun, C., Dunn, M. D., Reed, D. S. & Klimstra, W. B. Rational design of a live-attenuated Eastern equine encephalitis virus vaccine through informed mutation of virulence determinants. PLoS Pathog. 15, e1007584 (2019).
-
Tucker, P. C. & Griffin, D. E. Mechanism of altered Sindbis virus neurovirulence associated with a single-amino-acid change in the E2 glycoprotein. J. Virol. 65, 1551–1557 (1991).
-
Wang, E. et al. Chimeric Sindbis/Eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine 25, 7573–7581 (2007).
-
Plante, K. et al. Novel chikungunya vaccine candidate with an IRES-based attenuation and host range alteration mechanism. PLoS Pathog. 7, e1002142 (2011).
-
Roques, P. et al. Attenuated and vectored vaccines protect nonhuman primates against chikungunya virus. JCI Insight 2, e83527 (2017).
-
Robinson, D. M., Cole, F. E. Jr, McManus, A. T. & Pedersen, C. E. Jr. Inactivated Mayaro vaccine produced in human diploid cell cultures. Mil. Med. 141, 163–166 (1976).
-
Tiwari, M. et al. Assessment of immunogenic potential of Vero adapted formalin inactivated vaccine derived from novel ECSA genotype of chikungunya virus. Vaccine 27, 2513–2522 (2009).
-
Akahata, W. et al. A virus-like particle vaccine for epidemic chikungunya virus protects nonhuman primates against infection. Nat. Med. 16, 334–338 (2010).
-
Goo, L. et al. A virus-like particle vaccine elicits broad neutralizing antibody responses in humans to all chikungunya virus genotypes. J. Infect. Dis. 214, 1487–1491 (2016).
-
Ko, S. Y. et al. A virus-like particle vaccine prevents equine encephalitis virus infection in nonhuman primates. Sci. Transl. Med. https://doi.org/10.1126/scitranslmed.aav3113 (2019).
-
Brandler, S. et al. A recombinant measles vaccine expressing chikungunya virus-like particles is strongly immunogenic and protects mice from lethal challenge with chikungunya virus. Vaccine 31, 3718–3725 (2013).
-
Ramsauer, K. et al. Immunogenicity, safety, and tolerability of a recombinant measles-virus-based chikungunya vaccine: a randomised, double-blind, placebo-controlled, active-comparator, first-in-man trial. Lancet Infect. Dis. 15, 519–527 (2015).
-
Wang, D. et al. A complex adenovirus vaccine against chikungunya virus provides complete protection against viraemia and arthritis. Vaccine 29, 2803–2809 (2011).
-
Henning, L., Endt, K., Steigerwald, R., Anderson, M. & Volkmann, A. A monovalent and trivalent MVA-based vaccine completely protects mice against lethal Venezuelan, Western, and Eastern equine encephalitis virus aerosol challenge. Front. Immunol. 11, 598847 (2020).
-
Tatsis, N. et al. Adenoviral vectors persist in vivo and maintain activated CD8+ T cells: implications for their use as vaccines. Blood 110, 1916–1923 (2007).
-
Chang, L. J. et al. Safety and tolerability of chikungunya virus-like particle vaccine in healthy adults: a phase 1 dose-escalation trial. Lancet 384, 2046–2052 (2014).
-
Chen, G. L. et al. Effect of a chikungunya virus-like particle vaccine on safety and tolerability outcomes: a randomized clinical trial. JAMA 323, 1369–1377 (2020).
-
Reisinger, E. C. et al. Immunogenicity, safety, and tolerability of the measles-vectored chikungunya virus vaccine MV-CHIK: a double-blind, randomised, placebo-controlled and active-controlled phase 2 trial. Lancet 392, 2718–2727 (2019).
-
Folegatti, P. M. et al. A single dose of ChAdOx1 Chik vaccine induces neutralizing antibodies against four chikungunya virus lineages in a phase 1 clinical trial. Nat. Commun. 12, 4636 (2021).
-
Paessler, S. & Weaver, S. C. Vaccines for Venezuelan equine encephalitis. Vaccine 27, D80–D85 (2009).
-
Pierson, B. C. et al. Safety and immunogenicity of an inactivated Eastern equine encephalitis virus vaccine. Vaccine 39, 2780–2790 (2021).
-
Rappuoli, R. Reverse vaccinology. Curr. Opin. Microbiol. 3, 445–450 (2000).
-
Santiago, C. et al. Structures of T cell immunoglobulin mucin receptors 1 and 2 reveal mechanisms for regulation of immune responses by the TIM receptor family. Immunity 26, 299–310 (2007).
-
Sasaki, T. et al. Structural basis for Gas6-Axl signalling. EMBO J. 25, 80–87 (2006).
-
Soumahoro, M. K. et al. The chikungunya epidemic on La Réunion Island in 2005–2006: a cost-of-illness study. PLoS Negl. Trop. Dis. 5, e1197 (2011).
-
Feldstein, L. R. et al. Estimating the cost of illness and burden of disease associated with the 2014-2015 chikungunya outbreak in the U.S. Virgin Islands. PLoS Negl. Trop. Dis. 13, e0007563 (2019).
-
Semenza, J. C. & Menne, B. Climate change and infectious diseases in Europe. Lancet Infect. Dis. 9, 365–375 (2009).
-
Tsetsarkin, K. A., Vanlandingham, D. L., McGee, C. E. & Higgs, S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 3, e201 (2007).
-
Suhrbier, A. Rheumatic manifestations of chikungunya: emerging concepts and interventions. Nat. Rev. Rheumatol. 15, 597–611 (2019).
Acknowledgements
The authors thank J. Fox for insightful discussions and comments. Research in the authors’ laboratories was supported by US NIH grants R01 AI143673, U19 AI142790, R01 AI164653, R01 AI141436 and R01 AI127513 (to M.S.D.), and T32 AI172293 (to A.S.K.). A.S.K. acknowledges support from Open Philanthropy and the Life Sciences Research Foundation.
Author information
Authors and Affiliations
Contributions
A.S.K. and M.S.D. contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
M.S.D. is a consultant for Inbios, Vir Biotechnology, Senda Biosciences, Moderna, and Immunome. The Diamond laboratory has received unrelated funding support in sponsored research agreements from Vir Biotechnology, Moderna, Immunome and Emergent BioSolutions. A.S.K. declares no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, A.S., Diamond, M.S. A molecular understanding of alphavirus entry and antibody protection. Nat Rev Microbiol (2022). https://ift.tt/qyiMY1H
-
Accepted:
-
Published:
-
DOI: https://ift.tt/qyiMY1H
"entry" - Google News
December 06, 2022 at 09:59PM
https://ift.tt/bnmYxAB
A molecular understanding of alphavirus entry and antibody protection - Nature.com
"entry" - Google News
https://ift.tt/7JRp4ZF
https://ift.tt/eIX9jA0
Bagikan Berita Ini














0 Response to "A molecular understanding of alphavirus entry and antibody protection - Nature.com"
Post a Comment